-
Understanding the Risks and Symptoms of Penile Cancer

Cancerous cells are abnormal cells that grow in an uncontrolled manner. Eventually, the mass of abnormal cells can form a tumor. Cancerous cells can also spread well beyond their point of origin, making treatment more complicated and less likely to result in a favorable outcome. For these reasons, it’s important for men to understand their risk factors of cancers such as penile cancer , which originates at the penis. Another cornerstone of being a proactive patient is learning to recognize the potential signs of a urology health issue and seeking medical evaluations promptly.
Risk Factors
Risk factors can refer to anything that raises the risk of developing a certain disease. It’s important to bear in mind that having one or more risk factors of penile cancer does not mean that this cancer will definitely develop. Similarly, it’s possible to develop penile cancer without having risk factors for it. That said, knowing your risk factors can be helpful because this knowledge may guide your lifestyle choices and medical care. Smoking, for example, is one risk factor of penile cancer. Penile cancer is also associated with human papillomavirus (HPV) infection, HIV/AIDS infection, and a combination treatment for psoriasis that involves a medication and UV light treatment. Men who are uncircumcised are also at a higher risk of penile cancer.
Signs and Symptoms
If any unusual changes of the reproductive organs are noted, it’s advisable to seek a medical evaluation. Even if these abnormalities are not caused by penile cancer, they may be indicative of another medical condition that requires treatment. Men with penile cancer will most often notice changes in the skin on the penis, usually on the tip, but sometimes on the shaft. A lump, reddish rash, bleeding sore, and thickened or discolored skin could indicate penile cancer. Other signs include small bumps, bluish-brown growths, and swelling. If the cancer has already begun to spread, the lymph nodes in the groin area may become swollen.
Receiving a cancer diagnosis is devastating, but there is specialized cancer treatment available in Nashville. At Urology Associates, P.C., our urology team is committed to applying the latest medical technology and techniques to support optimal outcomes for our patients. Patients diagnosed with penile, testicular, or prostate cancer can contact us at (855) 901-1338 to request a consult.
-
The Link Between PSA Levels and Prostate Cancer
In men, the prostate gland produces a protein called prostate-specific antigen (PSA). A PSA test measures the level of this protein in a man’s bloodstream. This is clinically significant because prostate cancer can be associated with elevated PSA levels. However, it’s important to note that many men with prostate cancer do not have elevated PSA levels and many men with high PSA levels do not have prostate cancer. A urology specialist will evaluate each patient on a case-by-case basis.
You can learn more about PSA levels and prostate cancer by watching this video. This urology specialist explains the other exams that a man might have when prostate cancer is suspected, such as a digital rectal exam and a prostate biopsy.
If you have been referred to a prostate cancer specialist and you live in Nashville, you can call Urology Associates, P.C. at (855) 901-1338. Our urology team can answer any questions you may have about your elevated PSA levels .
-
Opening Up About OAB [INFOGRAPHIC]
Overactive bladder, or OAB, is an extremely common condition that affects millions of men and women in America. OAB is marked by urgency, urge incontinence, an increase in the frequency of urination, and waking at least two times per night to urinate. It can affect every part of your life and lead to social isolation and anxiety. Fortunately, your urologist has a number of remedies that can resolve your OAB and help you get back to living your life. Find out more about OAB in this Infographic from Urology Associates, P.C . Our urologists in Nashville treat a wide range of conditions, from OAB to UTIs and low libido. If you’re experiencing symptoms of OAB, don’t suffer in silence. Schedule a consultation with one of our specialists to find out how we can help. Please share this information to help others living with OAB and its troubling symptoms.

-
What Causes Pelvic Organ Prolapse?
Pelvic organ prolapse (POP) is a common urologic condition in which one of the pelvic organs moves out of position. For example, the bladder may drop lower and push against the vaginal walls. POP can cause uncomfortable symptoms, including pain or pressure in the area, incontinence, and constipation. If you suspect you might have POP, consider visiting a urology specialist to determine the underlying cause and learn about your treatment options.
Childbirth
Childbirth is among the most common causes of POP. To understand how childbirth can cause POP, it’s helpful to have a basic understanding of the anatomy in this area. POP can affect one or multiple organs, including the bladder, vagina, uterus, and rectum. These pelvic organs are normally held in place by the pelvic floor muscles. But these pelvic floor muscles can sometimes be stretched and weakened, which impairs their ability to hold the organs in place. Childbirth is a traumatic event that requires considerable straining and places significant pressure on the abdomen. The strain can weaken these crucial muscles.
Hysterectomy
Some women who undergo a hysterectomy will later develop POP. A hysterectomy is a surgical procedure to remove one or more of the pelvic organs such as the uterus. In the absence of these organs, the structures that are left intact may shift out of place. Although POP is not inevitable after a hysterectomy, this surgery is certainly a major risk factor for it.
Obesity
Not all cases of POP can be linked to childbirth and hysterectomies. The pelvic organs may also shift out of place due to the pressure exerted on the region by excessive body weight. Specifically, obesity results in increased pressure to the pelvic floor muscles, which can allow hernias to form. In other words, the bladder or other organs may prolapse into the vaginal wall.
Urology Associates, P.C. provides compassionate and confidential care for women with urologic and sexual health conditions, including pelvic organ prolapse. Call our office at (855) 901-1338 to request an appointment with a urologist in Nashville. Additional health information is available on our website.
-
What Does It Mean to Have an Elevated PSA?
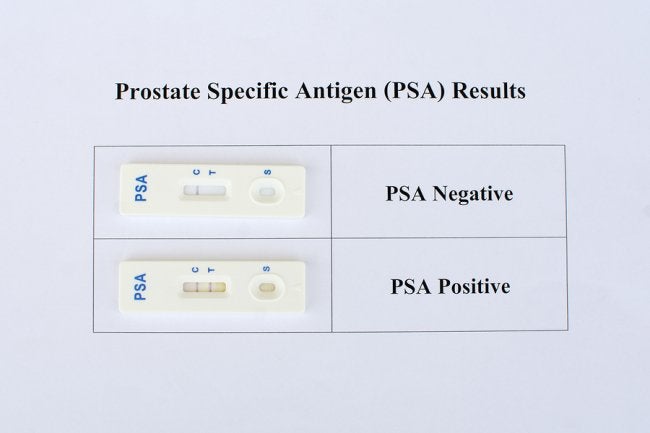
Prostate-specific antigen, or PSA, is a protein that is made by the prostate and present in your blood. Your primary care physician or urologist may perform a PSA test as a routine part of your preventative health care regime. Abnormal levels can indicate a health problem, such as prostate cancer.
If elevated PSA levels are detected during a blood test, your urologist may recommend further prostate cancer screening tests to determine if cancer could be the cause. It is important to note that elevated PSA levels do not necessarily mean that cancer is present, and normal PSA levels do not mean that no cancer exists. It is one tool in the cancer screening process that your urologist can use to detect the disease in early stages, when cancer treatment is most effective.
Your urologist at Urology Associates, P.C. will review all of your lab results with you, so you understand what things like elevated PSA levels mean for your overall health. To schedule an appointment for prostate cancer screenings in Nashville , please call (855) 901-1338.
-
A Look at Stress Urinary Incontinence
Urologists often diagnose stress urinary incontinence in women. It occurs when small amounts of urine leak at inappropriate times. Incontinence can occur when a person is sneezing, laughing, coughing, or engaging in any other activities that exert pressure on the bladder.
Watch this animation to learn more about why stress urinary incontinence occurs. It explains the basic anatomy of the area, such as the functions of the sphincters and pelvic floor muscles. In women, stress urinary incontinence is often the result of the weakening of the pelvic floor muscles after pregnancy and childbirth.
Effective treatments for incontinence are available in Tennessee. Contact Urology Associates, P.C. at (855) 901-1338 to request an appointment with a urologist.
-
Treating Recurrent Vaginal Yeast Infections

Women typically treat vaginal yeast infections with over-the-counter (OTC) products, assuming that there is no need to visit a urologist. However, women who develop recurrent yeast infections would be wise to see a urology specialist instead of continuing to rely on OTC suppositories. This is because it’s possible for these patients to actually have vestibulitis, which mimics the symptoms of vaginal yeast infections and may be caused by repeated yeast infections.
Vestibulitis is a chronic inflammatory problem that causes symptoms like burning, irritation, the frequent urge to urinate, and pain that occurs with pelvic pressure or vaginal entry. The treatment for this condition may involve medicated topical applications and lifestyle modifications, such as avoiding the exposure of chemical irritants. For example, women may be advised to avoid OTC vaginal products, scented laundry detergent, and douching.
At Urology Associates, P.C., women will find comprehensive and compassionate sexual health care in Nashville. Call us at (855) 901-1338 today or visit us online to learn about the conditions we treat , including sexual dysfunction.
-
Get the Facts About Chronic Testicular Pain

Thousands of men visit a urologist because of testicular pain. In some cases, the pain is caused by a debilitating condition called chronic testicular pain, or CTP. CTP ranges from mild to severe and can interfere with every day activities. If you believe you could be suffering from CTP, your urologist can provide treatments to ease your symptoms and help you enjoy a better quality of life. Here is what you need to know about this painful condition.
CTP may be constant or intermittent.
The discomfort associated with CTP may be constant in some men, while others have pain that comes and goes. The distinguishing factor between CTP and other types of testicular pain is that CTP persists for three months or more. Some men may have a sudden onset of pain that is eventually diagnosed as CTP, while others have pain that develops gradually.
Symptoms of CTP can vary.
Some men with CTP have symptoms all the time, but other men only have discomfort during activities. The pain can feel like aching and pressure or burning and throbbing and may also spread to the lower back and upper thighs. The pain can appear in one or both testicles and may switch from side to side. In some men, the pain is accompanied by swelling, fever, painful urination, painful intercourse or ejaculation, and bloody urine. Nausea and vomiting are also possible.
Several treatment options are available.
If you are diagnosed with CTP, the first thing you urologist will do is try to pinpoint the cause. Trauma, infections, hernias, cysts, and torsion are all potential causes of CTP, though in some cases, the cause is unknown. If your urologist does find a cause, treating the underlying issue can often resolve the CTP. Medications and surgery may be necessary to treat CTP.
Visit Urology Associates, P.C. for diagnosis and treatment any time you experience testicular pain. Our doctors provide comprehensive care for CTP , sexual health issues including erectile dysfunction, and testicular cancer in Nashville. To make your appointment, call (855) 901-1338.
-
Advice for Discussing Sexual Health Issues with Your Partner

If you or your partner is experiencing sexual health issues, such as erectile dysfunction or low libido, communication is an essential part of overcoming them. It’s not always easy to begin a conversation about sexual health, but it’s important for your relationship to have an open and ongoing dialogue with your partner about issues you may both be experiencing. These tips for discussing sexual health can help you start the conversation.
Pick the Right Time and Place
Because sexual health can be a sensitive topic, choose the time and place of your conversation wisely. Pick a time when you and your partner can sit together without distractions and aren’t rushed. Have your conversation in a private place, where both of you can feel comfortable talking about the issues openly and honestly. Avoid starting the conversation before work, when you have someplace to be, or otherwise have obligations that could interfere with your ability to talk for as long as you need to.
Be Direct
Be direct with your partner about your concerns about your sexual health and how it is or could affect your relationship. If have been diagnosed with a problem by your urologist, it can helpful to explain your condition and even give your partner materials your doctor may have provided to help you understand it. If your partner is the one experiencing the issue, ask any questions you may have and offer to research the answers together. The more informed both of you are about the issues, the better equipped you will be to face them together.
Talk About Treatments
Help your partner understand the treatment options available for the sexual health issue you are experiencing or ask questions about the treatments he or she is considering. In many cases, partner involvement in treatments can be helpful. In all cases, having the support of your partner when dealing with sexual health issues is important.
Your urologist at Urology Associates, P.C. can help you prepare for your conversation about sexual health by equipping you with the information you need. If you are experiencing sexual dysfunction in Nashville, make an appointment with a urologist today by calling (855) 901-1338.
-
What Are the Symptoms, Causes, and Treatments of Vaginal Atrophy?

Atrophic vaginitis, or vaginal atrophy , is a condition that urologists most often diagnose in women who are already in menopause, but it may also occur at other stages of a woman’s life. Vaginal atrophy is characterized by the thinning and inflammation of the tissues in the vaginal wall, which can cause painful symptoms and sexual dysfunction. Although these issues can be distressing, women should be aware that effective medical treatments are available.
Signs and Symptoms
Vaginal atrophy is a common cause of vaginal dryness, burning, itching, and unusual discharge. Many women also experience urinary symptoms, such as having the urgent need to urinate. A burning sensation may occur with urination and women may develop urinary incontinence. A patient’s history may reflect the increased occurrence of urinary tract infections (UTIs). Sexual intercourse can become uncomfortable or painful and some women may notice light bleeding or spotting afterward. As a result of these problems, it’s not unusual for women with vaginal atrophy to experience sexual dysfunction such as the loss of libido and orgasm problems. Marital distress may develop.
Causes and Risk Factors
The underlying cause of vaginal atrophy is a reduction in estrogen levels, which is why the condition most often affects post-menopausal women and those who are in perimenopause. A substantial decline in estrogen levels may also occur as a result of the surgical removal of the ovaries, cancer treatments, or breastfeeding. Certain factors may increase the risk of vaginal atrophy, including smoking, the lack of sexual activity, and the absence of vaginal births in the patient’s medical history.
Treatment Options
Hormone replacement therapy (HRT) is one option for restoring hormonal balance, but it’s generally advisable to consider other treatments first due to the risks of HRT. Women with mild vaginal atrophy may get good results with vaginal moisturizers and water-based lubricants. Women with more severe symptoms might consider drug-free laser therapy, which can provide relief after the first treatment.
The Women’s Institute for Sexual Health (WISH) at Urology Associates, P.C. connects women to caring urology specialists. We treat every patient with the utmost care to sensitivity and confidentiality. If you are experiencing a sexual health problem and live in Nashville, contact us today at (855) 901-1338.
Recent Posts
categories
- Uncategorized
- Bladder Cancer
- Women's Sexual Health
- MonaLisa Touch
- Urology
- Urologist
- Erectile Dysfunction
- Kidney Cancer
- Incontinence
- Prostate
- MonaLisa Touch Laser Treatment
- Kidney Stones
- Urinary Tract Infections
- Event
- Sexual Dysfunction
- Testicular Cancer
- Prostate Cancer
- Urology Surgery Center
- urinary incontinence
- vaginismus
- noncoital pain disorder
- Hypoactive Sexual Desire Disorder
- Infographic
- provenge
- Xofigo
- robotic surgery
- hormone replacement
- diabetes
- renal cell carcinoma
- pelvic pain
- hematuria
- sexual health
- chronic testicular pain
- premature ejaculation
- Men's Health Clinic
- Dr. Melvin Seard
- Interstitial Cystitis
- vasectomy
- overactive bladder
- vaginal atrophy
- nocturia
- bladder infections
- urethral strictures
- Acute Epididymitis
- low sex drive
- circumcision
- pelvic floor dysfunction
- Peyronie's Disease
- prostatitis
- female sexual dysfunction
- varicocele
- difficult urination
- low libido
- PSA levels
- male fertility
- penile prosthesis
- prostatic intraepithelial neoplasia
- male infertility
- estrogen levels
- nurse navigator
- stress urinary incontinence
- vaginal yeast infection
- elevated psa
- painful sex
- adult circumcision
- epididymitis
- OAB
- kidney infection
- penile cancer
- pelvic organ prolapse
- Vasectomy Reversal
- bone health
- cystectomies
- clinical trials
- bloody urine
- Advanced Therapeutic Center
- WISH MedSpa
- neurogenic bladder
- WISH Team
- prostate biopsies
- BPH
- fecal incontinence
- lithotripsy
- osteoporosis
- kidney cysts
